CD20
| MS4A1 | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | MS4A1, B1, Bp35, CD20, CVID5, LEU-16, MS4A2, S7, membrane spanning 4-domains A1, FMC7 | ||||||||||||||||||||||||||||||||||||||||||||||||||
| External IDs | OMIM: 112210; MGI: 88321; HomoloGene: 7259; GeneCards: MS4A1; OMA:MS4A1 - orthologs | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
B-lymphocyte antigen CD20 or CD20 is B lymphocyte cell-surface molecule.
It is a 33-37 kDa non-glykosylated protein. CD20 is expressed on the surface of B-cells from the pre-B phase, the expression is lost in terminally differentiated plasma cells.[5][6]
CD20 is used as a therapeutical target of B-cell malignancies and autoimmune diseases.[6]
Gene[edit]
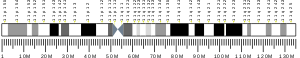
In humans CD20 is encoded by the MS4A1 gene localized to 11q12.[7][8]
The gene is 16 kbp long and consists of 8 exons. There are at least 3 mRNA transcripts (resulting from alternative splicing), that are all translated into an identical full-lenght CD20 protein product.[6][8] Variants 1 and 2 are poorly translated due to inhibitory upstream open reading frames and stem-loop structures within their 5' untranslated regions. The relative abundance of translation-competent variant 3, as opposed to the poorly translated variants 1 and 2, may be a key determinant of CD20 levels in normal and malignant human B cells and their responses to CD20-directed immunotherapies.[9]
MS4A1 gene is a member of the membrane-spanning 4A gene family. Members of this nascent protein family are characterized by common structural features and similar intron/exon splice boundaries and display unique expression patterns among hematopoietic cells and non-lymphoid tissues.[8]
Structure[edit]
CD20 is a transmembrane protein consisting of four hydrophobic transmembrane domains, one intracellular domain and two extracellular loops. There are three different forms of CD20 according to variable phosphorylation.
CD20 is located on the cell surface as homo-dimeric and homo-tetrameric oligomers. It is associated with other cell-surface and cytoplasmic proteins connected to the signal transduction (CD53, CD81, CD82).
CD20 is also known to be physically coupled to major histocompatibility complex class II (MHCII), CD40 and B-cell receptor (BCR).[6]
Function[edit]
The biological function of CD20 as well as its natural ligand is not fully elucidated.[6][10]
CD20 deletion in mice does not impair B-cell differentiation, isotype switch, maturation, proliferation or tissue localization. However, CD20−/− mice show decreased humoral immunity responses in both T-cell dependent and T-cell independent manner.[6]
Functional studies suggest that CD20 molecule is required for efficient BCR signaling. It possibly acts as a calcium channel (CD20 has structural similarities with some known ion channels) or is directly connected to calcium flux.
It is not fully understood, if other molecular pathways or B and T-cell interactions might be affected by CD20 levels on the B-cell surface.[6][11]
Expression[edit]
CD20 is expressed on all stages of B cell development from pre-B cells in the bone-marrow through immature, naive, mature and memory cells in lymphoid tissues and blood. The expression is lost on plasma blasts and plasma cells.[12][13]
CD20 is a marker of B cell malignancies. It is found on B-cell lymphomas, hairy cell leukemia, B-cell chronic lymphocytic leukemia, and melanoma cancer stem cells.[14]
Immunohistochemistry can be used to determine the presence of CD20 on cells in histological tissue sections. Because CD20 remains present on the cells of most B-cell neoplasms, and is absent on otherwise similar appearing T-cell neoplasms, it can be very useful in diagnosing conditions such as B-cell lymphomas and leukaemias.
However, the presence or absence of CD20 in such tumours is not relevant to prognosis, with the progression of the disease being much the same in either case. CD20 positive cells are also sometimes found in cases of Hodgkins disease, myeloma, and thymoma.[15]
Even though B cells represent the majority of CD20+ cells, a subset of CD3+ T cells also expresses CD20. CD20+ T cells are mostly CD8+ effector memory T cells with proinflammatory features. Further work is needed to understand the contribution of these cells to immune responses.[16]
Anti-CD20 monoclonal antibodies[edit]
The targeting of CD20 molecule is highly effective way to deplete B-cell populations.[11] Thus, anti-CD20 monoclonal antibodies (mAbs) play a crucial role in the management of B cell malignancies as well as some inflammatory and autoimmune diseases. The first anti-CD20 mAb approved by FDA in 1997 was Rituximab, defining a new epoch in hematooncology.
The advantages of CD20 as a therapeutic target are:
- conserved expresssion CD20 is expressed on the surface of virtually all mature B-cells. The expression on malignous B-cells is also relatively constant.
- limited off-target toxicity Anti-CD20 therapy does not affect hematopoietic stem cells and plasma cells, since they do not express CD20. It is important for B-cell repopulation following the therapy and retaining humoral protection against previously encountered pathogens via plasma cells, respectively.
- epitope stability The extracellular loops of CD20 are conserved sequences and undergo only a little post-translational modifications. It provides stable and predictable binding epitopes for mAbs.
Mechanism[edit]
Mechanism of action of anti-CD20 effects include:[11][17]
- Complement dependent cytotoxicity Anti-CD20 mAbs interact with C1q complement protein, leading to classical complement pathway activation and eventual complement dependent cytotoxicity.
- Fcγ receptor mediated effects Fcγ receptors expressed on neutrophils, NK cells or macrophages interact with Fc part of anti-CD20 mAb. The interaction leads to enhanced cytotoxic activity of NK cells (antibody-dependent cell-mediated cytotoxicity) and phagocytosis by macrophages and neutrophils (antibody-dependent cell-mediated phagocytosis).
- Hyper-crosslinking The accumulation of anti-CD20 mAbs on the cell surface may cause caspase-dependent apoptotic cell death.
In clinical practise[edit]
Examples of anti-CD20 mAbs and their approval status:[17]
| Generic name | Format | Indication | Approval status
(FDA/EMA) |
|---|---|---|---|
| Rituximab | chimeric IgG1 | NHL | 1998/1997 |
| Ibritumomab | mouse IgG1 | NHL | 2002/2004 |
| Ofatumumab | human IgG1 | CLL | 2009/2009 |
| Obinutuzumab | humanized IgG1 | CLL | 2013/2014 |
| Ocrelizumab | humanized IgG1 | MS | 2017/under review |
| Veltuzumab | humanized IgG1 | NHL, CLL, ITP | clinical trials |
| Ublituximab | chimeric IgG1 | CLL, MS | clinical trials |
| Ocaratuzumab | humanized IgG1 | CLL | clinical trials |
CD20 is the target of the mAbs rituximab, ocrelizumab, obinutuzumab, ofatumumab, ibritumomab tiuxetan, tositumomab, and ublituximab, which are all active agents in the treatment of all B cell lymphomas, leukemias, and B cell-mediated autoimmune diseases.
The anti-CD20 mAB ofatumumab (Genmab) was approved by FDA in October 2009 for chronic lymphocytic leukemia.
The anti-CD20 mAB obinutuzumab (Gazyva) was approved by FDA in November 2013 for chronic lymphocytic leukemia.
Ocrelizumab was approved by the FDA in March 2017 for multiple sclerosis as the first treatment of the primary progressive form of MS. Clinical trials in rheumatoid arthritis and systemic lupus erythematosus were discontinued in 2010 due to an infection related safety risk.[18]
Although phase II trials for the use of Rituximab in myalgic encephalomyelitis showed promising results, these could not be replicated in a large randomized controlled trial [19] and preliminary results from a Phase III trial were negative.[20]
Additional anti-CD20 antibody therapeutics under development (phase II or III clinical trials in 2008) include :
- Obinutuzumab for systemic lupus erythematosus,
- Ocaratuzumab for follicular lymphoma and rheumatoid arthritis,
- TRU-015 (by Trubion), (discontinued in 2010[21])
- IMMU-106 (veltuzumab).[22] for non-Hodgkin's lymphoma or (2015) immune thrombocytopenia.
Clinical significance[edit]
Diabetes mellitus[edit]
A link between the immune system's B cells and diabetes mellitus has been determined.[23]
In cases of obesity, the presence of fatty tissues surrounding the body's major organ systems results in cell necrosis and insulin insensitivity along the boundary between them. Eventually, the contents of fat cells that would otherwise have been digested by insulin are shed into the bloodstream. An inflammation response that mobilizes both T and B cells results in the creation of antibodies against these cells, causing them to become less responsive to insulin by an as-yet-unknown mechanism and promoting hypertension, hypertriglyceridemia, and arteriosclerosis, hallmarks of the metabolic syndrome.
Obese mice administered anti-B cell CD-20 antibodies, however, did not become less responsive to insulin and as a result, did not develop diabetes mellitus or the metabolic syndrome, the posited mechanism being that anti-CD20 antibodies rendered the T cell antibodies dysfunctional and therefore powerless to cause insulin insensitivity by a B cell antibody-modulated autoimmune response. The protection afforded by anti-CD-20 lasted approximately forty days—the time it takes the body to replenish its supply of B cells—after which repetition was necessary to restore it. Hence, it has been argued that diabetes mellitus be reclassified as an autoimmune disease rather than a purely metabolic one and focus treatment for it on immune system modulation.[24]
References[edit]
- ^ a b c GRCh38: Ensembl release 89: ENSG00000156738 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000024673 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Hardy R (2008). "Chapter 7: B Lymphocyte Development and Biology". In Paul W (ed.). Fundamental Immunology (Book) (6th ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 237–269. ISBN 978-0-7817-6519-0.
- ^ a b c d e f g Pavlasova G, Mraz M (June 2020). "The regulation and function of CD20: an "enigma" of B-cell biology and targeted therapy". Haematologica. 105 (6): 1494–1506. doi:10.3324/haematol.2019.243543. PMC 7271567. PMID 32482755.
- ^ Tedder TF, Streuli M, Schlossman SF, Saito H (January 1988). "Isolation and structure of a cDNA encoding the B1 (CD20) cell-surface antigen of human B lymphocytes". Proceedings of the National Academy of Sciences of the United States of America. 85 (1): 208–212. Bibcode:1988PNAS...85..208T. doi:10.1073/pnas.85.1.208. PMC 279513. PMID 2448768.
- ^ a b c "Entrez Gene: MS4A1 membrane-spanning 4-domains, subfamily A, member 1".
- ^ Ang Z, Paruzzo L, Hayer KE, Schmidt C, Torres Diz M, Xu F, et al. (November 2023). "Alternative splicing of its 5'-UTR limits CD20 mRNA translation and enables resistance to CD20-directed immunotherapies". Blood. 142 (20): 1724–1739. doi:10.1182/blood.2023020400. PMC 10667349. PMID 37683180. S2CID 261620430.
- ^ Cragg MS, Walshe CA, Ivanov AO, Glennie MJ (2005). "The biology of CD20 and its potential as a target for mAb therapy". B Cell Trophic Factors and B Cell Antagonism in Autoimmune Disease. Current Directions in Autoimmunity. Vol. 8. pp. 140–74. doi:10.1159/000082102. ISBN 978-3-8055-7851-6. PMID 15564720.
- ^ a b c Casan JM, Wong J, Northcott MJ, Opat S (2 December 2018). "Anti-CD20 monoclonal antibodies: reviewing a revolution". Human Vaccines & Immunotherapeutics. 14 (12): 2820–2841. doi:10.1080/21645515.2018.1508624. PMC 6343614. PMID 30096012.
- ^ Walport M, Murphy K, Janeway C, Travers PJ (2008). Janeway's Immunobiology (7th ed.). New York: Garland Science. ISBN 978-0-8153-4123-9.
- ^ Bonilla FA, Bona CA (1996). "5". Textbook of Immunology. Boca Raton: CRC. p. 102. ISBN 978-3-7186-0596-5.
- ^ Fang D, Nguyen TK, Leishear K, Finko R, Kulp AN, Hotz S, et al. (October 2005). "A tumorigenic subpopulation with stem cell properties in melanomas". Cancer Research. 65 (20): 9328–9337. doi:10.1158/0008-5472.CAN-05-1343. PMID 16230395.
- ^ Cooper K, Anthony Leong AS-Y (2003). Manual of diagnostic antibodies for immunohistology (2nd ed.). London: Greenwich Medical Media. ISBN 978-1-84110-100-2.
- ^ de Sèze J, Maillart E, Gueguen A, Laplaud DA, Michel L, Thouvenot E, et al. (23 March 2023). "Anti-CD20 therapies in multiple sclerosis: From pathology to the clinic". Frontiers in Immunology. 14: 1004795. doi:10.3389/fimmu.2023.1004795. PMC 10076836. PMID 37033984.
- ^ a b Marshall MJ, Stopforth RJ, Cragg MS (4 October 2017). "Therapeutic Antibodies: What Have We Learnt from Targeting CD20 and Where Are We Going?". Frontiers in Immunology. 8: 1245. doi:10.3389/fimmu.2017.01245. PMC 5632755. PMID 29046676.
- ^ "Roche and Biogen Idec Announce Their Decision to Discontinue the ocrelizumab Clinical Development Programme in Patients with Rheumatoid Arthritis". investors.biogen.com. Retrieved 6 January 2022.
- ^ Fluge Ø, Rekeland IG, Lien K, Thürmer H, Borchgrevink PC, Schäfer C, et al. (May 2019). "B-Lymphocyte Depletion in Patients With Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Randomized, Double-Blind, Placebo-Controlled Trial". Annals of Internal Medicine. 170 (9): 585–593. doi:10.7326/M18-1451. PMID 30934066. S2CID 91186383.
- ^ "ME-studie med negative resultater". Dagens Medicin (in Norwegian). Retrieved 6 January 2022.
- ^ "Trubion announces Pfizer's decision to discontinue development of TRU-015 for RA". Trubion Pharmaceuticals, Inc. press release. 15 June 2010.
- ^ Note: information included in this article only found in table present in print version of article. Morrow Jr KJ (15 June 2008). "Methods for Maximizing Antibody Yields". Genetic Engineering & Biotechnology News. Mary Ann Liebert, Inc. p. 36. Archived from the original on 13 February 2009. Retrieved 6 July 2008.
- ^ Winer DA, Winer S, Shen L, Wadia PP, Yantha J, Paltser G, et al. (May 2011). "B cells promote insulin resistance through modulation of T cells and production of pathogenic IgG antibodies". Nature Medicine. 17 (5): 610–617. doi:10.1038/nm.2353. PMC 3270885. PMID 21499269.
- Krista Conger (17 April 2011). "Type-2 diabetes linked to autoimmune reaction in study". Stanford School of Medicine. Archived from the original on 6 May 2011.
- ^ "Diabetes Mellitus". The Lecturio Medical Concept Library. Retrieved 9 July 2021.
Further reading[edit]
- Macardle PJ, Nicholson IC (2003). "CD20". Journal of Biological Regulators and Homeostatic Agents. 16 (2): 136–138. PMID 12144126.
- Tamayose K, Sato N, Ando J, Sugimoto K, Oshimi K (December 2002). "CD3-negative, CD20-positive T-cell prolymphocytic leukemia: case report and review of the literature". American Journal of Hematology. 71 (4): 331–335. doi:10.1002/ajh.10224. PMID 12447967. S2CID 23999423.
- Küster H, Zhang L, Brini AT, MacGlashan DW, Kinet JP (June 1992). "The gene and cDNA for the human high affinity immunoglobulin E receptor beta chain and expression of the complete human receptor". The Journal of Biological Chemistry. 267 (18): 12782–12787. doi:10.1016/S0021-9258(18)42344-7. PMID 1535625.
- Einfeld DA, Brown JP, Valentine MA, Clark EA, Ledbetter JA (March 1988). "Molecular cloning of the human B cell CD20 receptor predicts a hydrophobic protein with multiple transmembrane domains". The EMBO Journal. 7 (3): 711–717. doi:10.1002/j.1460-2075.1988.tb02867.x. PMC 454379. PMID 2456210.
- Tedder TF, Disteche CM, Louie E, Adler DA, Croce CM, Schlossman SF, et al. (April 1989). "The gene that encodes the human CD20 (B1) differentiation antigen is located on chromosome 11 near the t(11;14)(q13;q32) translocation site". Journal of Immunology. 142 (7): 2555–2559. doi:10.4049/jimmunol.142.7.2555. PMID 2466898. S2CID 20030567.
- Tedder TF, Klejman G, Schlossman SF, Saito H (April 1989). "Structure of the gene encoding the human B lymphocyte differentiation antigen CD20 (B1)". Journal of Immunology. 142 (7): 2560–2568. doi:10.4049/jimmunol.142.7.2560. PMID 2466899. S2CID 30587436.
- Loken MR, Shah VO, Dattilio KL, Civin CI (November 1987). "Flow cytometric analysis of human bone marrow. II. Normal B lymphocyte development". Blood. 70 (5): 1316–1324. doi:10.1182/blood.V70.5.1316.1316. PMID 3117132.
- Stamenkovic I, Seed B (June 1988). "Analysis of two cDNA clones encoding the B lymphocyte antigen CD20 (B1, Bp35), a type III integral membrane protein". The Journal of Experimental Medicine. 167 (6): 1975–1980. doi:10.1084/jem.167.6.1975. PMC 2189672. PMID 3260267.
- Bofill M, Janossy G, Janossa M, Burford GD, Seymour GJ, Wernet P, et al. (March 1985). "Human B cell development. II. Subpopulations in the human fetus". Journal of Immunology. 134 (3): 1531–1538. doi:10.4049/jimmunol.134.3.1531. PMID 3871452. S2CID 29484405.
- Deans JP, Kalt L, Ledbetter JA, Schieven GL, Bolen JB, Johnson P (September 1995). "Association of 75/80-kDa phosphoproteins and the tyrosine kinases Lyn, Fyn, and Lck with the B cell molecule CD20. Evidence against involvement of the cytoplasmic regions of CD20". The Journal of Biological Chemistry. 270 (38): 22632–22638. doi:10.1074/jbc.270.38.22632. PMID 7545683.
- Valentine MA, Licciardi KA, Clark EA, Krebs EG, Meier KE (January 1993). "Insulin regulates serine/threonine phosphorylation in activated human B lymphocytes". Journal of Immunology. 150 (1): 96–105. doi:10.4049/jimmunol.150.1.96. PMID 7678037. S2CID 24522632.
- Bubien JK, Zhou LJ, Bell PD, Frizzell RA, Tedder TF (June 1993). "Transfection of the CD20 cell surface molecule into ectopic cell types generates a Ca2+ conductance found constitutively in B lymphocytes". The Journal of Cell Biology. 121 (5): 1121–1132. doi:10.1083/jcb.121.5.1121. PMC 2119683. PMID 7684739.
- Shirakawa T, Li A, Dubowitz M, Dekker JW, Shaw AE, Faux JA, et al. (June 1994). "Association between atopy and variants of the beta subunit of the high-affinity immunoglobulin E receptor". Nature Genetics. 7 (2): 125–129. doi:10.1038/ng0694-125. PMID 7920628. S2CID 24026689.
- Maruyama K, Sugano S (January 1994). "Oligo-capping: a simple method to replace the cap structure of eukaryotic mRNAs with oligoribonucleotides". Gene. 138 (1–2): 171–174. doi:10.1016/0378-1119(94)90802-8. PMID 8125298.
- Szepetowski P, Perucca-Lostanlen D, Gaudray P (June 1993). "Mapping genes according to their amplification status in tumor cells: contribution to the map of 11q13". Genomics. 16 (3): 745–750. doi:10.1006/geno.1993.1257. PMID 8325649.
- Algino KM, Thomason RW, King DE, Montiel MM, Craig FE (July 1996). "CD20 (pan-B cell antigen) expression on bone marrow-derived T cells". American Journal of Clinical Pathology. 106 (1): 78–81. doi:10.1093/ajcp/106.1.78. PMID 8701937.
- Szöllósi J, Horejsí V, Bene L, Angelisová P, Damjanovich S (October 1996). "Supramolecular complexes of MHC class I, MHC class II, CD20, and tetraspan molecules (CD53, CD81, and CD82) at the surface of a B cell line JY". Journal of Immunology. 157 (7): 2939–2946. doi:10.4049/jimmunol.157.7.2939. PMID 8816400. S2CID 18389389.
- Kanzaki M, Lindorfer MA, Garrison JC, Kojima I (June 1997). "Activation of the calcium-permeable cation channel CD20 by alpha subunits of the Gi protein". The Journal of Biological Chemistry. 272 (23): 14733–14739. doi:10.1074/jbc.272.23.14733. PMID 9169438.
- Suzuki Y, Yoshitomo-Nakagawa K, Maruyama K, Suyama A, Sugano S (October 1997). "Construction and characterization of a full length-enriched and a 5'-end-enriched cDNA library". Gene. 200 (1–2): 149–156. doi:10.1016/S0378-1119(97)00411-3. PMID 9373149.
External links[edit]
- CD20+antigen at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- representations of the shape are found here and more detail here
- Human MS4A1 genome location and MS4A1 gene details page in the UCSC Genome Browser.
- Human MS4A2 genome location and MS4A2 gene details page in the UCSC Genome Browser.