User:Mr. Ibrahem/Peripheral neuropathy
| Peripheral neuropathy | |
|---|---|
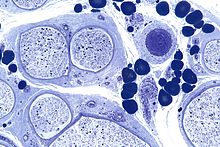 | |
| Micrograph showing a vasculitic peripheral neuropathy; plastic embedded; Toluidine blue stain | |
| Specialty | Neurology |
| Symptoms | Sensory: Numbness, neuropathic pain, poor balance[1] Motor: Muscle weakness, twitching, muscle shinking[1] Autonomic: Trouble with heat, excess sweating, trouble swallowing[1] |
| Types | Predominantly sensory, predominantly motor, sensory-motor, and autonomic neuropathy[1] |
| Causes | Diabetic neuropathy, alcoholic neuropathy, Guillain-Barré syndrome, carpal tunnel syndrome, meralgia paresthetica, complex regional pain syndrome, injury, poor blood flow, autoimmune, kidney or liver problems, vitamin B12 deficiency, paraneoplastic syndromes, certain medications including chemotherapy, genetics, shingles, Lyme disease, HIV/AIDS, unclear[1][2] |
| Diagnostic method | Based on symptoms, examination, and blood tests[1] |
| Treatment | Based on underlying cause, nortriptyline, duloxetine, gabapentin[1] |
| Frequency | 1 to 7% of people[2] |
Peripheral neuropathy, sometimes shortened to neuropathy, is damage to peripheral nerves, meaning nerves that connect the brain and spinal cord to the rest of the body.[1] Symptoms depend on the type of nerves involved.[1] This may include muscle weakness, twitching, or shinking; numbness, neuropathic pain, or poor balance; or trouble with heat, excess sweating, or trouble swallowing.[1] Onset may be over days to years.[1] It often starts with the lower legs and hands.[2]
Common types include diabetic neuropathy, alcoholic neuropathy, Guillain-Barré syndrome, carpal tunnel syndrome, meralgia paresthetica, and complex regional pain syndrome.[1][2] Other causes include injury, poor blood flow, autoimmune, kidney or liver problems, vitamin B12 deficiency, vitamin B6 deficiency, paraneoplastic syndromes, certain medications including chemotherapy, genetics, shingles, Lyme disease, and HIV/AIDS; though the cause may remain unclear.[1][2] Diagnosis is based on symptoms and examination.[1] Blood tests are generally done for diabetes, vitamins, liver, thyroid, and kidney function; while tests for abnormal proteins may also be done.[1][2] Other tests may include nerve conduction velocity, electromyography, or nerve biopsy.[1]
If the underlying cause can be address, recovery may occur over time.[1] Other measures that may help include stopping smoking, exercise, and blood sugar control.[1] Autoimmune cases may be improved with medications such as prednisone, cyclosporine, or azathioprine.[1] Plasmapheresis may also help in certain cases.[1] Medications to improve pain may include nortriptyline, duloxetine, or gabapentin.[1]
Peripheral neuropathy affects about 1 to 7% of people.[2] This includes up to half of people with diabetes.[2] It becomes more common over the age of 50.[2] Clear descriptions of the condition date from 1880 by Joseph Jules Dejerine.[3]
References[edit]
- ^ a b c d e f g h i j k l m n o p q r s t u "Peripheral Neuropathy". National Institute of Neurological Disorders and Stroke. Archived from the original on 26 August 2023. Retrieved 23 September 2023.
- ^ a b c d e f g h i Castelli, G; Desai, KM; Cantone, RE (15 December 2020). "Peripheral Neuropathy: Evaluation and Differential Diagnosis". American family physician. 102 (12): 732–739. PMID 33320513.
- ^ Ouvrier, Robert A.; Ouvrier, Robert; Mcleod, J. G.; Pollard, J. D. (1999). "1. Historical perspective: overview of paediatric aspects of the neuropathies". Peripheral Neuropathy in Childhood. Cambridge University Press. p. 1. ISBN 978-1-898683-17-9. Archived from the original on 20 October 2023. Retrieved 23 September 2023.
